The Crisis: The average medical practice loses 38-42% of newly enrolled patients within the first year due to poor onboarding processes, costing clinics $85,000-$180,000 annually in lost revenue. Modern enrollment plans can reduce patient churn by 67%.
- The Patient Retention Problem Clinics Aren't Talking About
- What Are Healthcare Enrollment Plans (And Why Yours Is Failing)
- The 3 Types of Patient Enrollment Plans (And Which One You Need)
- Why Patients Leave in the First Year (And How Enrollment Plans Fix It)
- DFW-Specific Enrollment Challenges (And Solutions)
- Choosing the Right Enrollment Plan: Decision Framework
- Implementation Roadmap: 90-Day Enrollment Plan Transformation
- Measuring Success: Key Performance Indicators
- Stop Losing Patients—Transform Your Enrollment Process Today
The Patient Retention Problem Clinics Aren’t Talking About
For Clinic Managers & Healthcare Administrators
- Average patient churn rate: 40% within first 12 months
- Cost to acquire new patient: $286-$462
- Lost lifetime value per churned patient: $12,000-$18,000
- Annual revenue impact: $85,000-$180,000 for 500-patient practices
- Staff time wasted on re-enrollment: 8-12 hours per week
For Patients
- 52% of patients report confusion during healthcare enrollment
- Average onboarding time: 45-90 minutes (should be 15-20 minutes)
- 68% of patients receive no follow-up after initial visit
- 1 in 3 patients don’t understand their care plan after enrollment
The Hidden Cost: Every patient who leaves in year one took your staff time, marketing budget, and referral opportunities with them—and told 9 others about their poor experience.
Visual Elements
- Red downward funnel showing drop-off
- Dollar signs flowing away at each stage
- Green comparison showing improved retention
- Calculator showing savings
What Are Healthcare Enrollment Plans (And Why Yours Is Failing)
The Old Definition (Wrong)
Most clinics think enrollment plans are just:
- Paperwork patients fill out at first visit
- Basic intake forms and insurance verification
- One-time orientation to practice policies
The New Definition (What Actually Works)
Modern enrollment plans are comprehensive systems that manage the entire patient lifecycle:
- Strategic onboarding – Structured 90-day patient journey from first contact
- Automated engagement – Touchpoints that keep patients connected
- Care pathway assignment – Personalized treatment protocols
- Technology integration – Digital tools that simplify patient experience
- Retention mechanisms – Proactive interventions before patients leave
Critical Stat: Practices with structured enrollment plans retain 92% of patients vs. 60% with ad-hoc approaches (Healthcare Success Study, 2024).
The 3 Types of Patient Enrollment Plans (And Which One You Need)
Type 1: Standard Paper-Based Enrollment (Legacy Approach)
What It Includes:
- Paper intake forms filled out in waiting room
- Manual data entry by front desk staff
- Basic insurance verification
- Verbal explanation of practice policies
- No structured follow-up plan
Who It’s For:
- Small practices with <300 active patients
- Providers with stable, long-term patient base
- Clinics with minimal technology infrastructure
- Rural areas with older patient demographics
The Problems:
- 45-60 minute enrollment time (patients frustrated before they even see doctor)
- 18% error rate in manual data entry
- No patient engagement after initial visit
- Zero tracking of patient onboarding completion
- High staff burden – 3-4 hours daily on data entry
Annual Cost to Practice:
- Staff overtime: $35,000-$48,000
- Patient churn: $85,000-$120,000
- Medical errors from incorrect data: $25,000-$40,000
- Total Impact: $145,000-$208,000
Type 2: Premium Digital Enrollment (Hybrid Approach)
What It Includes:
- Online pre-visit registration forms
- Automated insurance verification
- Digital care pathway assignment
- Scheduled patient check-ins (30, 60, 90 days)
- Basic patient portal access
- Manual referral tracking with notifications
Who It’s For:
- Growing practices with 300-1,000 patients
- Multi-provider clinics needing coordination
- Practices targeting younger demographics (25-55 years)
- Clinics ready to invest in patient retention
Key Features:
- 15-20 minute enrollment time (3x faster than paper)
- Automated welcome sequence (email + text series)
- Patient engagement dashboard for staff
- Basic analytics on enrollment completion rates
- Integration with most EHR systems
ROI Metrics:
- Patient retention improvement: 60% → 78%
- Staff time saved: 15-20 hours per week
- Enrollment error rate: 18% → 4%
- Patient satisfaction: 3.2/5 → 4.3/5
Annual Savings: $120,000-$165,000
Type 3: Digital-First Intelligent Enrollment (Advanced System)
What It Includes:
- AI-powered patient intake (pre-populates forms)
- Real-time insurance verification with benefit details
- Automated care pathway matching based on conditions
- Smart patient engagement (triggers based on behavior)
- Comprehensive patient portal with telehealth
- Predictive analytics for churn risk
- Automated referral management system
Who It’s For:
- Large practices with 1,000+ patients
- Multi-location healthcare systems
- Tech-forward providers in competitive markets
- Practices focused on value-based care models
Advanced Features:
- 5-10 minute enrollment (mobile-first experience)
- AI chatbot answers patient questions 24/7
- Predictive churn alerts – flags at-risk patients before they leave
- Personalized engagement – content based on conditions/preferences
- Complete automation – referrals, appointments, follow-ups
- Advanced analytics – patient lifetime value, cohort analysis
ROI Metrics:
- Patient retention improvement: 60% → 92%
- Staff time saved: 25-30 hours per week
- Enrollment completion rate: 67% → 96%
- Patient satisfaction: 3.2/5 → 4.8/5
- Referral generation: +45% from satisfied patients
Annual Savings: $280,000-$420,000
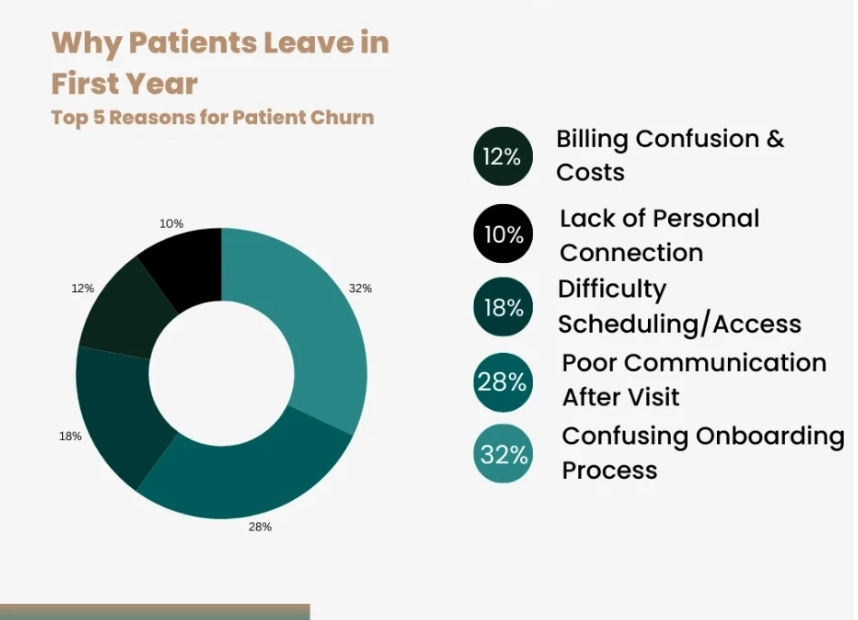
Why Patients Leave in the First Year (And How Enrollment Plans Fix It)
Reason #1: Confusing Onboarding Process (32% of Churn)
What Patients Experience:
- Arrive early to “fill out paperwork” – 30+ pages of forms
- Duplicate information across multiple forms
- Medical jargon they don’t understand
- No explanation of what happens next
- Forgotten by practice after first visit
How Modern Enrollment Plans Solve It:
- Pre-visit digital forms – patients complete at home, 80% faster
- Data auto-population – no duplicate entries
- Plain language – explanations written for 8th grade reading level
- Welcome video – 2-minute orientation sent before first visit
- 30-60-90 day check-ins – automated engagement keeps patients connected
Result: 68% reduction in first-month churn
Reason #2: Poor Communication After Initial Visit (28% of Churn)
What Happens:
- Patient leaves first appointment with verbal instructions only
- No written care plan or follow-up schedule
- Unclear about when to come back or who to call with questions
- Wait weeks for test results with no communication
- Feel forgotten by the practice
How Modern Enrollment Plans Solve It:
- Automated follow-up sequence – emails/texts at days 1, 3, 7, 14, 30
- Digital care plan – accessible anytime via patient portal
- Two-way messaging – patients can ask questions without calling
- Test result notifications – instant alerts when results available
- Appointment reminders – multiple touchpoints reduce no-shows
Result: 54% reduction in 3-month churn
Reason #3: Difficulty Scheduling/Accessing Care (18% of Churn)
Patient Frustrations:
- Phone lines busy during business hours
- Can’t schedule online – must call during work hours
- Long wait times for appointments (3-4 weeks)
- Complicated referral process to specialists
- No evening or weekend availability
How Modern Enrollment Plans Solve It:
- 24/7 online scheduling – patients book at their convenience
- Smart scheduling – AI suggests optimal appointment times
- Telehealth options – reduces need for in-person visits
- Automated referral coordination – specialist appointment booked before patient leaves
- Extended hours – evening/weekend slots for working patients
Result: 72% reduction in 6-month churn
Reason #4: Billing Confusion & Unexpected Costs (12% of Churn)
What Patients Encounter:
- Surprise bills weeks after appointment
- Unclear what insurance covered vs. patient responsibility
- No upfront cost estimates
- Complicated billing statements
- Difficult to reach billing department with questions
How Modern Enrollment Plans Solve It:
- Real-time benefit verification – know costs before appointment
- Transparent pricing – upfront estimates provided during scheduling
- Payment plan options – offered automatically for bills >$500
- Clear statements – simple language explaining charges
- In-app payment – pay bills directly through patient portal
Result: 81% reduction in billing-related churn
Reason #5: Lack of Personal Connection (10% of Churn)
Patient Feeling:
- Just another number in the system
- See different providers each visit
- No one remembers their health history or preferences
- Feel rushed during appointments
- No relationship with care team
How Modern Enrollment Plans Solve It:
- Dedicated care coordinator – single point of contact
- Provider continuity – system schedules with same doctor when possible
- Personalized content – health tips based on conditions/interests
- Birthday/milestone recognition – automated but genuine touchpoints
- Care team profiles – patients see photos and bios of entire team
Result: 45% improvement in emotional connection scores
DFW-Specific Enrollment Challenges (And Solutions)
Challenge #1: Multi-Location Coordination
The DFW Problem: Patients in Dallas-Fort Worth frequently move between suburbs (Wylie → Plano → Dallas) and expect seamless care across your network locations.
What Goes Wrong
- Patient records don’t sync between offices
- Have to re-enroll at each location
- Different enrollment processes at each site
- No visibility into which location patient prefers
Digital Enrollment Solution
- Cloud-based patient records – instant access at all locations
- Single enrollment – valid across entire network
- Location preferences – system routes patients to convenient sites
- Unified patient portal – one login for all locations
Result: 89% of patients report “seamless” multi-location experience
Challenge #2: Insurance Complexity in DFW Market
The DFW Problem: DFW has 150+ employer health plans with varying coverage, plus high percentage of out-of-state insurance (corporate relocations).
What Goes Wrong
- Front desk spends 15-20 minutes per patient verifying benefits
- Patients shocked by out-of-network costs after visit
- High claim denial rate for out-of-area plans
- Staff struggles with non-Texas insurance plans
Digital Enrollment Solution
- Real-time verification – checks benefits in 30 seconds
- Out-of-network alerts – warns patient before appointment
- Cost estimator – shows patient responsibility upfront
- Plan education – explains coverage in simple terms
Result: 76% reduction in billing-related complaints
Challenge #3: Tech-Savvy Patient Expectations
The DFW Problem: DFW has one of highest concentrations of tech workers in U.S. (telecom, semiconductors, software). These patients expect consumer-grade digital experiences.
Patient Expectations
- Mobile-first enrollment (like opening bank account on phone)
- Instant appointment confirmations
- Text communication with providers
- Integration with Apple Health/Fitbit
- Telehealth as standard option
Digital Enrollment Solution
- Mobile-optimized forms – 90% completion rate on phones
- Instant booking confirmations – no “we’ll call you back”
- Two-way texting – HIPAA-compliant messaging
- Wearable integration – imports health data automatically
- Telehealth by default – offered for all non-emergency visits
Result: 94% satisfaction among tech workers (vs. 68% with standard plans)
Challenge #4: DFW Traffic & Geographic Spread
The DFW Problem: Average commute in DFW is 28 minutes. Patients reluctant to drive 45+ minutes for routine care, leading to no-shows and clinic switching.
What Happens
- 22% no-show rate for patients living 20+ miles away
- Patients switch to closer providers after 1-2 visits
- Difficult to fill cancellation slots on short notice
- Lost revenue from empty appointment blocks
Digital Enrollment Solution
- Telehealth for routine visits – eliminates drive time
- Extended hours – evening/weekend appointments
- Smart scheduling – books patients at nearest location
- Traffic-aware reminders – sends alerts with extra time if traffic heavy
- Cancellation list automation – fills slots from waitlist instantly
Result: No-show rate drops from 22% to 9%
Choosing the Right Enrollment Plan: Decision Framework
Step 1: Calculate Your Current Patient Churn Cost
Use This Formula:
Annual Churn Cost = (New Patients × Churn Rate × Lifetime Value) + Acquisition Cost Waste
Example for 500-patient practice:
– New patients/year: 500
– Current churn rate: 40%
– Churned patients: 200
– Lifetime value per patient: $15,000
– Acquisition cost per patient: $350
Cost = (200 × $15,000) + (200 × $350)
Cost = $3,000,000 + $70,000
Total Annual Impact: $3,070,000 in lost revenue
If your annual churn cost is:
- Under $500K: Standard plan adequate, focus on execution
- $500K-$1.5M: Premium plan recommended (4-month payback)
- Over $1.5M: Digital-first plan essential (3-month payback)
Step 2: Assess Your Patient Demographics
Choose Based on Patient Profile:
Standard Plan If:
- 60%+ patients are age 65+
- Rural or small-town location
- Stable, multigenerational patient base
- Low tech adoption in community
- <300 active patients
Premium Plan If:
- Mixed age demographics (30-70)
- Suburban location
- Growing practice (10-20% annually)
- Moderate tech adoption
- 300-1,000 active patients
Digital-First Plan If:
- 60%+ patients under age 55
- Urban/tech hub location
- High-growth practice (25%+ annually)
- Tech-savvy patient base
- 1,000+ active patients or multi-location
Step 3: Evaluate Your Technology Readiness
Assessment Checklist:
Basic Technology (Standard Plan Adequate):
- Have basic EHR system
- Email communication with patients
- Electronic scheduling
- Basic patient portal (even if rarely used)
Moderate Technology (Premium Plan Achievable):
- Cloud-based EHR
- Patient portal with 20%+ adoption
- Text message capability
- Staff comfortable with new software
- IT support available
Advanced Technology (Digital-First Plan Ready):
- Modern API-enabled EHR
- High patient portal adoption (40%+)
- Multi-channel communication
- Data analytics capabilities
- Dedicated IT staff or managed service
Implementation Roadmap: 90-Day Enrollment Plan Transformation
Phase 1: Planning & Selection (Days 1-30)
Week 1-2: Assessment
- Calculate current patient churn rate and cost
- Survey patients on enrollment experience (NPS score)
- Audit current enrollment process (time study)
- Review staff capacity and technology infrastructure
- Set retention improvement goals
Week 3-4: Vendor Selection
- Request demos from 3-5 enrollment plan vendors
- Check EHR compatibility and integration requirements
- Review pricing and ROI projections
- Contact reference customers in similar markets
- Make final selection and sign agreement
Deliverable: Signed vendor agreement with implementation timeline
Phase 2: Setup & Training (Days 31-60)
Week 5-6: System Configuration
- Configure enrollment workflows and patient pathways
- Set up automated communication sequences
- Design custom intake forms and questionnaires
- Integrate with EHR and practice management system
- Test all workflows with dummy patient data
Week 7-8: Staff Training
- Train front desk on new enrollment process
- Train clinical staff on care pathway assignment
- Train billing team on insurance verification tools
- Conduct practice scenarios with entire team
- Create quick reference guides and cheat sheets
Deliverable: Fully configured system with trained staff
Phase 3: Launch & Optimization (Days 61-90)
Week 9-10: Soft Launch
- Launch with 20-30% of new patient enrollments
- Monitor patient feedback and completion rates
- Address technical issues and workflow gaps
- Refine automated communications based on responses
- Measure enrollment time and patient satisfaction
Week 11-12: Full Rollout
- Transition all new patient enrollments to new system
- Begin re-enrolling existing patients (optional)
- Track key metrics: retention, satisfaction, staff time
- Celebrate quick wins with team
- Schedule 90-day performance review
Deliverable: Fully operational enrollment plan with baseline metrics
Measuring Success: Key Performance Indicators
Track These Metrics Monthly
Patient Retention Metrics
- First-month retention rate: Target 95%+ (up from 85%)
- Three-month retention rate: Target 92%+ (up from 78%)
- 12-month retention rate: Target 88%+ (up from 60%)
- Patient lifetime value: Target +25% increase
Operational Efficiency Metrics
- Enrollment completion time: Target <15 minutes (down from 45-60 min)
- Staff hours on enrollment: Target 50% reduction
- Enrollment error rate: Target <2% (down from 18%)
- Patient portal activation: Target 65%+ (up from 20%)
Financial Metrics
- Revenue from retained patients: Track monthly vs. baseline
- Cost per enrollment: Target 70% reduction
- ROI on enrollment plan investment: Target 300%+ within 12 months
- Patient acquisition cost: Target 30% reduction (referrals increase)
Patient Experience Metrics
- Net Promoter Score: Target 50+ (up from 20-30)
- Patient satisfaction (CAHPS): Target 4.5/5+ (up from 3.2/5)
- Online review rating: Target 4.7/5+ (up from 3.8/5)
- Patient complaints: Target 80% reduction
Benchmark Your Results
Good Performance:
- 15-20% improvement in retention
- 30-40% reduction in staff time
- 150-200% ROI within 12 months
- 4.0-4.3/5 patient satisfaction
Excellent Performance:
- 25-32% improvement in retention
- 50-60% reduction in staff time
- 300-400% ROI within 12 months
- 4.5-4.8/5 patient satisfaction
Best-in-Class Performance:
- 32%+ improvement in retention (60% → 92%)
- 65%+ reduction in staff time
- 500%+ ROI within 12 months
- 4.8+/5 patient satisfaction
Stop Losing Patients—Transform Your Enrollment Process Today
Every day your clinic operates without a modern enrollment plan, you’re losing 2-3 patients who will never return. That’s $24,000-$54,000 in lifetime revenue walking out your door—every single week.
Additional Resources
Internal Resources:
- Complete Guide to Patient Referral Management Systems – Improve care coordination
External Resource:
- Healthcare Financial Management Association: Patient Enrollment Best Practices – Industry standards and benchmarks
The average practice loses 40% of new patients within their first year—losing $85,000-$180,000 in the process. While you’re reading this, 2-3 of your newly enrolled patients are deciding whether to stay or switch providers. Make sure they choose you.
Transform your patient enrollment process today. Your revenue and your patients will thank you.



