Medical billing in 2025 isn’t just changing, it’s being redefined. With hundreds of new CPT codes now in effect, even the most efficient practices could be at risk of revenue loss, compliance penalties, and patient dissatisfaction. The real question is: are you ready for the impact these updates will have on your practice?
- 2025 CPT Code Updates: What Healthcare Providers Need to Know
- Why Healthcare Providers Are Struggling with 2025 Medical Billing Updates
- 2025 CPT Code Changes: What's Actually Different (And Why It Matters to Your Revenue)
- The Telehealth Coding Revolution: New CPT Codes You Can't Afford to Miss
- New Mental Health CPT Codes for 2025
- DFW Healthcare Providers: Region-Specific Challenges You're Facing
- Wylie & DFW-Specific Coding Considerations
- Implementation Strategy: Your 90-Day Action Plan for Coding Updates
- Technology Solutions: How Automation Prevents Coding Errors
- Compliance & Audit Protection: Staying Safe in 2025
- Financial Impact: Real Numbers from Real Practices
- Practice Size Impact Analysis:
- Real-World Success Stories:
- Take Action Now: Don't Let 2025 Updates Drain Your Revenue
- Revenue Cycle Metrics After Implementation
- The Bottom Line: Invest in Accuracy or Pay in Denials
- Contact Integrate Point Wylie Today
2025 CPT Code Updates: What Healthcare Providers Need to Know
The clock struck midnight on January 1, 2025, and suddenly 270 new CPT codes went live—potentially affecting every claim your practice submits. For healthcare providers in Wylie, Texas, and across the nation, understanding these medical billing and coding updates isn’t just about compliance anymore; it’s about protecting your bottom line and ensuring patients receive proper care documentation.
The Reality Check: A recent MGMA study found that practices lose an average of $125,000 annually due to coding errors and outdated billing practices. With 2025’s massive overhaul—270 new codes, 112 deletions, and 38 revisions—the risk has never been higher.
Why Healthcare Providers Are Struggling with 2025 Medical Billing Updates
The Triple Threat Facing Your Practice
Impact on Healthcare Administrators & Billing Managers:
- Revenue leakage from incorrect code usage reaching 7-11% of potential collections
- Claim denial rates spiking by 23% in practices slow to adopt new coding standards
- Staff burnout as billing teams struggle with 420 total CPT changes implemented simultaneously
- Compliance penalties averaging $15,000-$50,000 per violation for systematic coding errors
Challenges for Physicians & Clinical Staff:
- Documentation requirements expanding by 30% for new telehealth and mental health codes
- Time spent on administrative tasks increasing while patient care time decreases Confusion about which codes apply to evolving treatment modalities
- Fear of audit triggers from incorrect code application
Consequences for Patients:
- Unexpected bills due to coding errors and claim denials
- Delays in treatment authorization when codes don’t match insurance requirements
- Confusion about coverage for telehealth and new service types
- Longer wait times as practices struggle with administrative bottlenecks
2025 CPT Code Changes: What’s Actually Different (And Why It Matters to Your Revenue)
Breaking Down the Numbers
The American Medical Association released these critical updates:
CPT Code Updates for 2025:
- 270 new CPT codes added (largest annual increase in 5 years)
- 112 CPT codes deleted (affecting commonly billed services)
- 38 codes revised with modified guidelines
- Impact: 15-20% of all practices will use at least one new code weekly
ICD-10-CM Diagnostic Code Changes:
- 252 new codes for enhanced diagnostic specificity
- 13 deletions of outdated diagnoses
- 36 revisions affecting chronic disease management
- Greater precision required for value-based reimbursement models
HCPCS Level II Updates:
- 309 new codes (primarily DME, prosthetics, orthotics)
- Critical for practices billing Medicare and Medicaid
- Expanded coverage for home health equipment and supplies
The Telehealth Coding Revolution: New CPT Codes You Can’t Afford to Miss
Why This Matters Now
Telehealth Coding
- 68% of providers now offer telehealth (up from 43% in 2020)
- Coding errors cost practices $8,000-$15,000 monthly
- Revenue opportunity: Proper coding captures an additional $2,400-$3,600 monthly for a 5-provider practice with 100 telehealth visits
New codes cover:
- Asynchronous telehealth (store-and-forward)
- Remote patient monitoring with clearer documentation
- Virtual check-ins and e-visits
- Mental health telehealth with substance abuse specificity
Required documentation:
- Platform used and security compliance
- Patient consent
- Time-based vs. complexity-based justification
- Geographic locations of provider and patient
- Medical appropriateness vs. in-person visit
Telehealth Billing Compliance Guide for Texas Providers →Virtual Assistants for Clinics: Boost Efficiency & Care
Mental Health Services
- Mental health visits increased 47% nationwide in 2024
- New codes enable $85-$175 per session reimbursement increase
- Crisis intervention, collaborative care, and substance use disorder codes now separately billable
New Mental Health CPT Codes for 2025
What’s Now Billable:
- Crisis intervention codes with time-based increments
- Collaborative care management for integrated behavioral health
- Psychiatric collaborative care with expanded billing periods
- Substance use disorder treatment codes (office and telehealth)
- Group therapy codes with revised participant requirements
Practice Impact for Wylie, Texas Providers:
- Mental health integration now viable for primary care practices
- Collaborative care models showing 32% higher patient retention
- Reimbursement rates competitive with traditional fee-for-service
- Documentation burden reduced compared to 2024 requirements
DFW Healthcare Providers: Region-Specific Challenges You’re Facing
Why Location Matters for Medical Billing Success
Texas Healthcare Landscape Data:
- 18.4% uninsured rate (highest among large states)
- Medicaid expansion not adopted, affecting reimbursement mix
- High Medicare Advantage penetration requiring different coding approaches
- Rapid population growth stressing existing provider networks
Wylie & DFW-Specific Coding Considerations
Insurance Mix Complexity:
- Major payers: Baylor Scott & White, UnitedHealthcare, Blue Cross Blue Shield Texas
- Medicare Advantage plans requiring different documentation than Traditional Medicare
- Each has unique coding requirements for pre-authorization
- Higher proportion of cash-pay patients needing accurate cost estimates
Patient Payment Solutions & Financial Counseling Services →Avoid Payment Penalties: Smart Billing Tips for Clinics 2025
Local Health Systems Impact:
- Network requirements affecting code selection for referrals
- UT Southwestern and Baylor affiliated practices have specific EMR coding workflows
- Children’s Health network codes pediatric services differently
- Texas Health Resources specific billing protocols
Growth-Related Pressures:
- 3.2% annual population increase creating capacity challenges
- Telehealth adoption essential for covering sprawling metro area
- Mental health demand outpacing provider availability
- Urgent care and retail clinic competition requiring billing efficiency
Implementation Strategy: Your 90-Day Action Plan for Coding Updates
Assessment – Days 1 to 30:
- Audit top 50 CPT codes currently billed
- Identify deleted codes still in use
- Calculate denial rates by payer
- Update EHR/practice management software
- Install 2025 CPT and ICD-10-CM updates
Training – Days 31 to 60:
- 8 hours mandatory training for billing staff
- 2 hours physician education on documentation
- Update clinical note templates
- Create specialty-specific quick-reference guides
- Results from structured training:
- 43% reduction in claim denials
- 28% faster claim processing
- $18,000 average monthly revenue increase
Launch & Optimize – Days 61 to 90:
- Daily claim reviews for first two weeks
- Weekly chart audits (10-15 charts minimum)
- Monitor denial patterns
- Track days in accounts receivable
Technology Solutions: How Automation Prevents Coding Errors
AI and automation reduce coding errors by 52%:
- Computer-assisted coding cuts lookup time by 40%
- Automated claim scrubbing reduces denials by 35-50%
- Real-time eligibility verification prevents non-covered service billing
ROI Example (10-provider practice, $15K investment):
- +$72,000 annual revenue from fewer denials
- 15 staff hours saved weekly
- 62% faster claim turnaround
- Payback in 2.5-4 months
For the most current official CPT code information, visit the American Medical Association CPT Updates Page
Compliance & Audit Protection: Staying Safe in 2025
The High Cost of Getting It Wrong
Audit Statistics That Should Concern You:
- 1 in 4 practices will face a payer audit in 2025
- Average cost of responding to audit: $25,000-$75,000
- Systematic coding errors can trigger 3-5 year lookback periods
- OIG work plan targets telehealth and mental health billing specifically
Building Your Compliance Shield
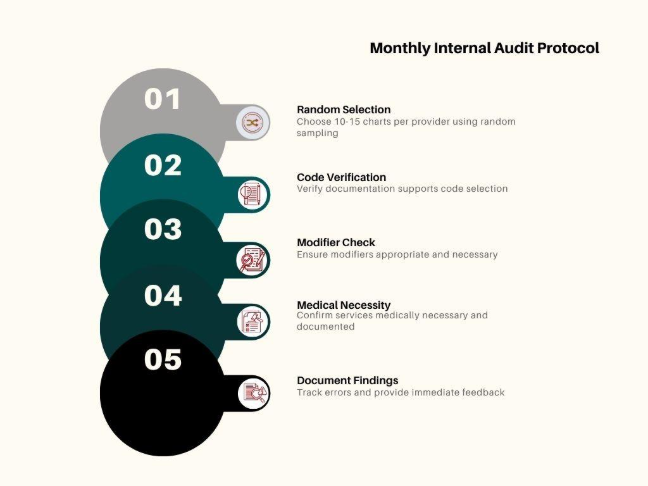
- Monthly Audit Protocol
- Review 10–15 charts per provider
- Prioritize new codes & high-value services
- Confirm documentation supports coding
- Verify modifier accuracy
- Ensure time-based codes include proper time details
- Validate medical necessity for all services
Red Flags for Audits
- Sudden coding pattern changes
- >60% high-level E/M codes
- Telehealth claims lacking documentation
- Unbundling services
- Use of deleted codes
- Missing or invalid modifiers
2025 Documentation Standards
- Clearly show clinical necessity in every note
- Telehealth: add required extra elements
- Mental health: include specific diagnostic criteria
- Time-based codes: record start/stop or total minutes
- Chronic care management: include full care plans
Case Study: A 7-provider family practice in Texas faced a $187,000 RAC audit demand due to telehealth coding errors. After implementing weekly internal audits and documentation training, they:
- Reduced audit risk by 78%
- Improved documentation quality scores from 6.2/10 to 9.1/10
- Successfully appealed $143,000 of the demand
- Established defensible billing practices going forward
Financial Impact: Real Numbers from Real Practices
What Proper 2025 Coding Implementation Actually Returns
Revenue Cycle Metrics That Improve:
| Metric | Before 2025 Update | After Proper Implementation | % Change |
| Clean Claim Rate | 82% | 94% | +15% |
| Days in A/R | 47 days | 32 days | -32% |
| Denial Rate | 9.2% | 3.8% | -59% |
| Collection Rate | 91% | 97% | +6.6% |
| Cost to Collect | $3.82 | $2.41 | -37% |
Practice Size Impact Analysis:
Small Practice (3-5 providers):
- Average monthly charges: $180,000
- Revenue loss from coding errors: $16,200-$19,800
- Potential recovery with 2025 updates: $12,000-$15,000 monthly
- Annual impact: $144,000-$180,000
Medium Practice (6-15 providers):
- Average monthly charges: $525,000
- Revenue loss from coding errors: $47,250-$57,750
- Potential recovery with 2025 updates: $35,000-$43,000 monthly
- Annual impact: $420,000-$516,000
Large Practice (16+ providers):
- Average monthly charges: $1,200,000+
- Revenue loss from coding errors: $108,000-$132,000
- Potential recovery with 2025 updates: $80,000-$98,000 monthly
- Annual impact: $960,000-$1,176,000
Real-World Success Stories:
We were skeptical about the ROI of updating our billing processes, but after implementing 2025 coding changes properly, our denial rate dropped from 11% to 4% in just two months. That’s $28,000 extra in collections monthly.
Practice Manager, 8-Provider Internal Medicine Group, Plano, TX
The telehealth codes alone generated an additional $4,200 monthly once we understood proper documentation. We were leaving money on the table every single day.
Billing Director, behavioral health practice, Dallas, TX
Take Action Now: Don’t Let 2025 Updates Drain Your Revenue
The difference between thriving and barely surviving in 2025’s healthcare landscape comes down to one thing: how quickly you adapt to these billing changes.
Your Next Steps (Choose Your Path):
Fast-Track Implementation (Recommended for Busy Practices)
Partner with medical billing experts who live and breathe these updates daily. Integrate Point Wylie specializes in:
- Complete 2025 coding transition management (we handle everything)
- Staff training programs customized to your specialty and EMR
- Ongoing compliance monitoring to protect against audits
- Revenue cycle optimization that increases collections by 15-30%
Schedule Your Free Consultation Now – Same-Week Appointments Available
DIY Approach (For Practices with Dedicated Billing Teams)
- Access our webinar library featuring specialty-specific coding updates
- Join our monthly billing Q&A sessions with certified coding specialists
- Subscribe to our weekly email updates on emerging coding issues
Not Sure Where You Stand? Take our 5-minute Billing Health Assessment to identify:
- Your current coding accuracy score
- Potential revenue gaps in your practice
- Top 3 areas for immediate improvement
- Customized recommendations based on your specialty
Revenue Cycle Metrics After Implementation
| Metric | Before | After | Improvement |
| Clean Claim Rate | 82% | 94% | +15% |
| Days in A/R | 47 days | 32 days | -32% |
| Denial Rate | 9.2% | 3.8% | -59% |
| Collection Rate | 91% | 97% | +6.6% |
| Cost to Collect | $3.82 | $2.41 | -37% |
The Bottom Line: Invest in Accuracy or Pay in Denials
Every day you delay 2025 medical billing and coding updates, you lose money. With 7–11% average revenue leakage, a $500,000/month practice risks $35,000–$55,000 in preventable losses.
The choice is simple:
Implement updates in 90 days with modest investment
Or face denied claims and compliance risks worth hundreds of thousands
Your patients deserve accuracy. Practice deserves full reimbursement. Your staff deserves clarity.
Contact Integrate Point Wylie Today
Special Offer for 2025: First 20 practices to schedule receive a complimentary comprehensive revenue cycle audit ($1,500 value) and customized 2025 implementation roadmap.
Integrate Point, Wylie provides comprehensive medical billing, coding, and revenue cycle management services to healthcare practices throughout the DFW metroplex. Our certified coding specialists stay current with all AMA, CMS, and payer-specific requirements to maximize your reimbursement and minimize compliance risk.