Ever been told you need prior authorization before a procedure and wondered what it really means? Whether it’s surgery, medication, or routine care, understanding this step can save patients money and providers time. Read on to uncover how the process works and how to avoid costly delays.
- Pre-Authorization Checklist: What You Need Before Your Procedure
- What is Prior Authorization?
- Why is Prior Authorization Important?
- The Prior Authorization Process
- How Long Does Prior Authorization Take?
- Common Types of Prior Authorization
- How to Prepare for Prior Authorization
- Special Considerations for DFW Area Patients
- What to Do If Your Prior Authorization Is Denied
- Medicare and Medicaid Prior Authorization
- Tips for a Smooth Prior Authorization Experience
- Understanding Precertification and Preauthorization
- Avoiding Preauthorization Penalties
- Conclusion
Pre-Authorization Checklist: What You Need Before Your Procedure
Navigating the prior authorization process can be overwhelming for patients and providers alike, but understanding what’s required before your procedure can save time, reduce stress, and help avoid costly delays. Whether you need prior authorization for surgery, medication prior authorization, or to complete a prior authorization form, understanding what is required before your procedure can save you time, reduce stress, and help avoid delays in your care.
What is Prior Authorization?
How does prior authorization work? Prior authorization is a process used by insurance companies to determine if a prescribed service, medication, or procedure is medically necessary before they agree to cover it. This step helps control costs and ensures patients receive appropriate care.
Sometimes called precertification or preauthorization for prescribed medications, prior authorization requires your healthcare provider to submit a request—often using a prior authorization form—to your insurance company. This process applies to many types of care, from surgeries to specialty medications and even some diagnostic tests.
Why is Prior Authorization Important?
Obtaining authorization in medical billing is crucial because it affects your insurance coverage and out-of-pocket costs. Without proper authorization in medical billing, patients may face claim denials, unexpected bills, or even a preauthorization penalty. Insurance companies use prior authorization criteria to decide if the procedure or medication is covered under your plan.
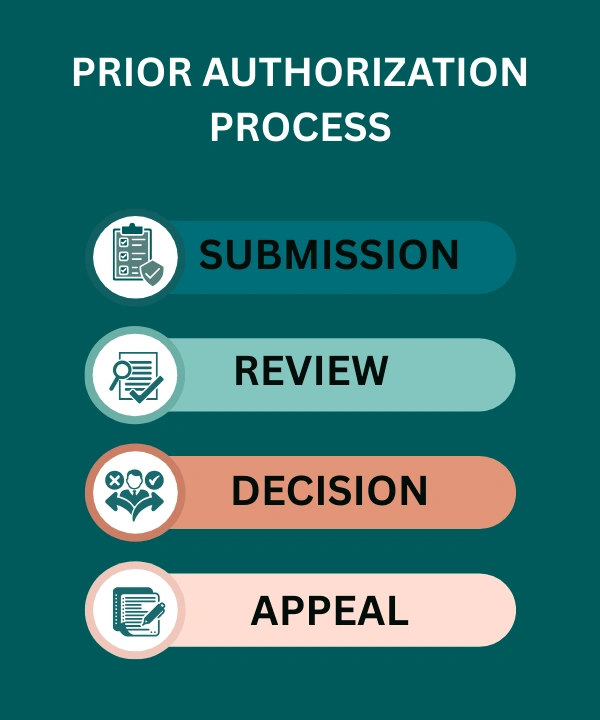
The Prior Authorization Process
The insurance preauthorization process typically involves several steps:
- Submission: Your healthcare provider submits a prior authorization request or prior auth forms to your insurance company.
- Review: The insurance company reviews the request based on their prior authorization criteria.
- Decision: You receive medication approval or denial.
- Appeal: If denied, you may need to appeal or provide additional information.
🔗 Learn more: Understanding Insurance Eligibility Verification
How Long Does Prior Authorization Take?
How long does prior authorization take? The timeline varies by insurance provider and the complexity of the procedure. It can take anywhere from a few hours to several days. For urgent cases, some insurers offer expedited reviews. Always start the process as soon as your provider recommends a procedure or medication to avoid delays.
Common Types of Prior Authorization
- Prior authorization for surgery: Surgeries often require prior approval to ensure medical necessity.
- Medication prior authorization and preauthorization letter for insurance: Many medications, especially specialty drugs, need prior authorization.
- Pharmacy prior authorization: Pharmacy-related approvals to confirm coverage for prescribed medications.
- Medicare prior authorization and Medicare prior authorization for medication: Medicare-specific authorization processes, often requiring a Medicare prior authorization form for providers.
- Medicaid preauthorization form: Medicaid-related forms and approvals, which may differ from private insurance requirements.
How to Prepare for Prior Authorization
- Ensure your healthcare provider completes the prior authorization form accurately.
- Provide all necessary medical records and documentation.
- Follow up with your provider and insurance company to check the status.
- Understand your insurance’s prior authorization certification and requirements.
- If using UnitedHealthcare, be aware of their specific United Healthcare authorizations process.
Special Considerations for DFW Area Patients
For Dallas patients and those throughout the DFW metroplex, understanding regional insurance patterns can be particularly helpful when navigating prior authorization. In the DFW area, many major health systems including Baylor Scott & White, Texas Health Resources, and Methodist Health System have established streamlined prior authorization processes with major insurers like Blue Cross Blue Shield of Texas, Aetna, and UnitedHealthcare.
Clinics in Texas often face unique challenges with prior authorization timelines due to the state’s large geographic area and diverse insurance networks. For Dallas patients, it’s especially important to verify that your chosen provider is in-network with your insurance plan, as out-of-network procedures may require additional authorization steps or result in higher out-of-pocket costs. Many DFW healthcare facilities offer dedicated prior authorization coordinators who are familiar with Texas-specific insurance requirements and can help expedite the approval process for local patients.
What to Do If Your Prior Authorization Is Denied
If you receive a prior authorization denied notice, don’t panic. You can:
- Request a detailed explanation from your insurer.
- Work with your provider to submit an appeal or additional documentation.
- Provide further medical information to support your case.
- Ask about alternative treatments that may not require preauthorization.
Medicare and Medicaid Prior Authorization
Specific rules apply for Medicare prior authorization and Medicaid. Providers often use a Medicare prior authorization form or Medicaid preauthorization form to facilitate the process. Patients should be aware of these requirements to avoid delays and ensure coverage for their procedures or medications.
Tips for a Smooth Prior Authorization Experience
- Start the process early to avoid delays.
- Keep copies of all submitted forms and correspondence.
- Communicate regularly with your healthcare provider and insurance company.
- Use prior authorization services or online portals to track and manage your requests.
- Confirm insurance approval before scheduling your procedure.
Understanding Precertification and Preauthorization
There is often confusion between preauthorization and precertification. While both involve getting insurance approval before a procedure, precertification is typically used for hospital admissions or certain outpatient services, while preauthorization can apply to medications, tests, and procedures. Always check your insurance plan to understand which process applies. Knowing the difference between preauthorization and precertification can help you avoid unnecessary delays or penalties.
Avoiding Preauthorization Penalties
Failure to obtain required preauthorization can lead to denied claims, higher out-of-pocket costs, or even full responsibility for the bill. Always confirm with your provider and insurance company that all necessary steps have been completed before your procedure.
To protect your practice from revenue loss, it’s important to understand how insurers evaluate claims and payments. Many penalties arise not from fraud, but from unintentional errors such as incorrect coding or missed follow-up visit rules. By following proper coding and billing guidelines, providers can avoid denials, ensure accurate reimbursement, and stay compliant with evolving payer requirements—especially under plans like Anthem Blue Cross Blue Shield in 2025.
Conclusion
Understanding the prior authorization process and preparing accordingly can make a significant difference in your healthcare journey. At Integrate Point, we are committed to helping you navigate these processes smoothly, ensuring you get the care you need without unnecessary delays.
If you have questions about how to do prior authorization or need assistance with insurance approval, contact Integrate Point for expert guidance and support. Our team is here to help you with every step, from obtaining the right forms to appealing denied requests—so you can focus on your health, not the paperwork.